Accurate medical billing depends on understanding and applying CPT codes correctly. Even a small mistake in coding can delay payments, increase denials, and create unnecessary stress for staff. One code that often raises questions is CPT 96372, which is used for therapeutic injections. For small practices and clinics, knowing when and how to bill this code is essential for keeping claims clean and revenue steady.
Here, we’ll look closely at what this CPT code covers, when it applies, what documentation payers expect, and the best ways to avoid common mistakes. We’ll also share tips on how medical billing services can support small practices with accurate injection claims.
What CPT Code 96372 Really Means
CPT 96372 is used when a healthcare provider administers a therapeutic, prophylactic, or diagnostic injection by intramuscular (IM) or subcutaneous (Sub-Q) route. Common examples include injections for antibiotics, steroids, hormone therapy, or pain relief.
It’s important to know exactly what this code represents before attaching it to a claim. Misuse of this code is one of the biggest reasons claims are denied.
When the Code Applies
This code is billed when the injection is given under a provider’s order and is not part of an immunization or chemotherapy treatment. For instance:
- A patient with an infection receives an IM antibiotic injection.
- A diabetic patient is given a Sub-Q hormone injection.
- A patient with a vitamin deficiency receives a B12 injection.
Each of these scenarios would qualify for CPT 96372 code.
What Does Not Qualify
Immunizations are billed under their own CPT codes, and infusions fall under a different set of billing CPT codes. Submitting this code for these services is considered incorrect coding and usually results in denials.
Why Documentation Matters for CPT 96372
Payers are strict about documentation because it proves medical necessity and service accuracy. Missing or incomplete notes are one of the fastest ways to lose revenue.
Essential Patient Details
Make sure every claim includes accurate demographic and insurance information. Even small errors in ID numbers or policy details can delay payment.
Clinical Justification and Diagnosis
Providers should always document the medical reason for the injection, supported by ICD-10 codes. Without this link, insurers may question the necessity of the procedure.
Tip: Always connect the 96372 code claim to the correct diagnosis code. For example, billing an antibiotic injection should be paired with a diagnosis for infection, not a vague symptom.
Recording the Injection
Notes should include:
- Date and time of service
- Site of injection (e.g., left arm, right thigh)
- Medication name, strength, dosage, and lot number
- The credentials of the person administering it
Providers must use structured templates in their EHR to ensure no details are left out. This also makes it easier for billing staff or an external medical billing services team to submit clean claims.
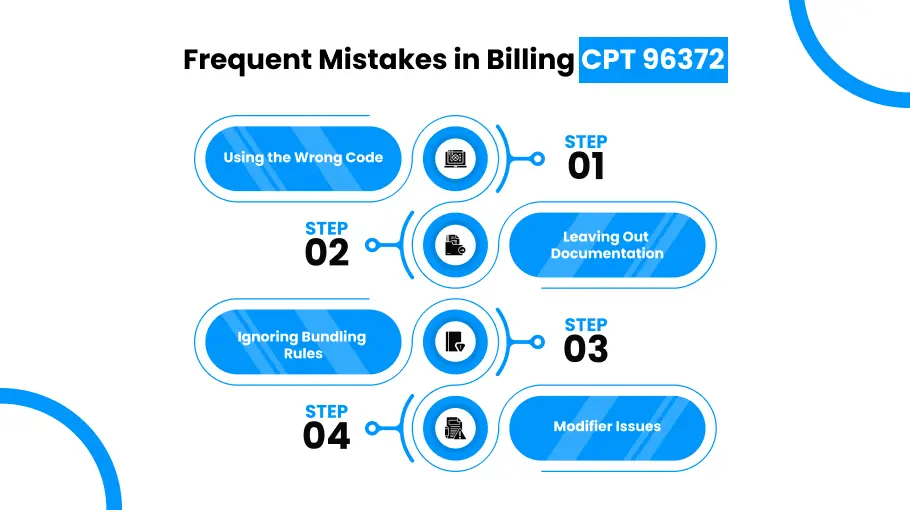
Frequent Mistakes in Billing CPT 96372
Billing errors create more work for staff and slow down revenue. Here are common mistakes to avoid:
- Using the Wrong Code
Practices often confuse 96372 with immunization codes or infusion codes. Always review payer guidance and compare with other billing CPT codes to ensure you’re selecting the right one.
- Leaving Out Documentation
Claims without physician orders or missing injection details (like route or dosage) are red flags for payers.
Tip: Conduct monthly audits to spot documentation gaps early.
- Ignoring Bundling Rules
Sometimes this code is bundled with another service. For example, if billed with an office visit, you may need modifier -25 to show the visit was a separate, medically necessary service.
- Modifier Issues
If multiple injections are given on the same day, modifiers may be required. Leaving these off can cause rejections.
Tip: Train your staff to recognize modifier requirements. Many billing and coding services provide checklists that make this step easier.
How to Bill CPT 96372 Correctly
Getting this code right the first time saves practices from endless rework and lost revenue.
- Pairing With the Right Diagnosis
Always connect 96372 to a diagnosis code that supports medical necessity. Example: pairing a B12 injection with an anemia diagnosis code.
- Billing the Drug Separately
Don’t forget that the injection administration and the drug are billed separately. Use HCPCS J-codes for the drug itself.
Keep a quick reference sheet of common J-codes used in your practice to avoid delays.
- Staff Training and Workflow Checklists
Every staff member who touches billing should know the basics of injection claims. Standardized checklists help reduce human error.
Reimbursement Considerations for CPT 96372
Knowing how payers reimburse this code helps practices set realistic expectations.
- It is typically reimbursed per injection, not per drug.
- Medicare and private insurers may have slightly different rules.
- Some payers limit how many times it can be billed in a single day.
Tips for Avoiding Denials With CPT 96372
Denials are costly, but most are preventable. Here are some tips to help you do that:
- Verify Coverage First
Check the patient’s insurance eligibility before giving the injection. This prevents denials caused by inactive or incomplete coverage.
- Keep Records Detailed and Consistent
Provider orders, injection details, and ICD-10 codes should all align. Inconsistent notes are a top reason payers deny claims.
- Use Technology Wisely
Many practices rely on billing software or support from billing and coding services to track claim status and receive alerts about potential errors.
- Audit Regularly
Set up internal or outsourced audits every quarter. This not only catches recurring mistakes but also improves compliance and staff training.
Conclusion
CPT 96372 may seem like a simple code, but billing it correctly requires attention to detail. Complete documentation, proper modifiers, and pairing with the right ICD-10 codes are all critical for clean claims. By building strong workflows and working with experts in medical billing services, practices can reduce denials, improve reimbursement rates, and keep their cash flow steady.
At the end of the day, accurate billing isn’t just about getting paid; it’s about creating reliable systems that support providers, staff, and patients alike.
At DoctorPapers, we specialize in helping healthcare providers across the US manage billing CPT codes and optimize revenue cycles. By entrusting your therapeutic injection billing to professionals, you protect your practice from denials, maximize reimbursements, and streamline your operations.
FAQs
- What are common mistakes when billing CPT 96372?
Errors include billing multiple injections incorrectly, confusing injection types, missing modifiers, and incomplete documentation.
- How is CPT 96372 different from CPT 96365?
CPT 96372 code is for subcutaneous or intramuscular injections, while CPT 96365 is used for intravenous (IV) infusion or push therapy.
- What documentation is required for CPT 96372?
Providers must document the patient’s details, medication name and dosage, route and site of administration, medical necessity, and their own signature to ensure claim approval.
- Can CPT 96372 be billed with an office visit?
Yes, but only when the evaluation and management (E/M) service is significant and separately identifiable. In those cases, modifier -25 should be added to the E/M code to show it was distinct from the injection administration.
- Is the medication included in CPT 96372 billing?
No. this code only covers the administration of the injection. The drug itself must be billed separately using the appropriate HCPCS J-code that matches the medication given.




![Cost of Hiring Virtual Medical Assistants in the USA [2026] Blog Banner](https://doctorpapers.com/wp-content/uploads/2025/12/Cost-of-Hiring-Virtual-Medical-Assistants-in-the-USA-2026-300x152.webp)
