When it comes to running a successful healthcare practice, nothing is more frustrating than having your hard-earned payments delayed, or worse, denied due to claim rejections. Every denied claim is more than just lost revenue; it’s additional staff time, higher operational costs, and unnecessary stress.
The good news? Most claim issues stem from a predictable set of problems that can be addressed with the right systems and expertise.
Let’s break down the most common errors that prevent clean claims, and explore how strategic medical billing solutions can keep your cash flow healthy.
Why Clean Claims Matter More Than Ever
A medical claim that is error-free and correctly processed by the payer on its initial submission is referred to as a “clean claim.” Clean claims in the United States are about speed as much as accuracy. The margin for error is decreasing due to stricter payer regulations, changing medical coding errors, and increasingly complicated compliance requirements.
Every denied claim means lost time, late payments, and possible compliance issues for healthcare providers. This is the point at which a successful billing plan supported by knowledgeable experts changes everything.
- Inaccurate Patient Demographics
It might sound simple, but even minor typos in a patient’s name, date of birth, or insurance ID can cause a claim to be rejected. For example: “Johnathan” vs. “Jonathan”, that single missing “h” could trigger an error in the payer’s system.
Solution: Implement verification procedures before submitting a claim and during check-in. Payer databases will precisely match your submission details if you use automated verification techniques.
- Medical Coding Errors
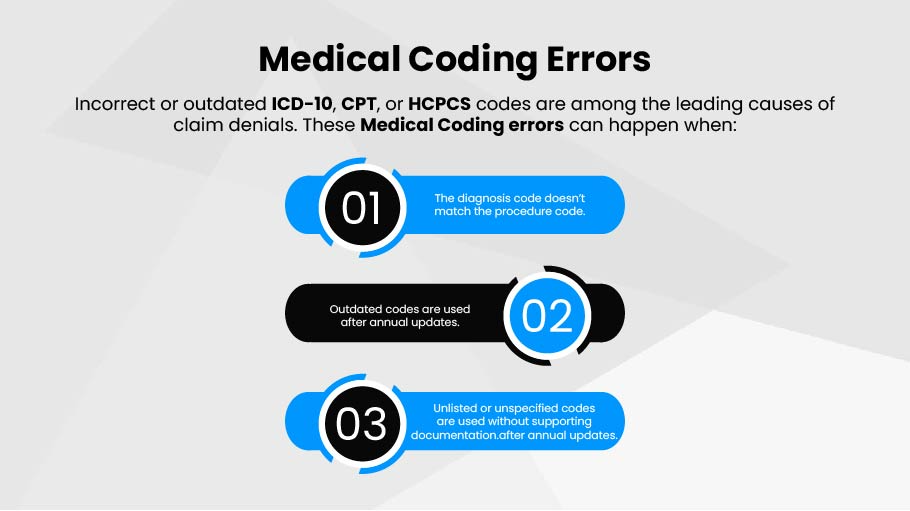
Incorrect or outdated ICD-10, CPT, or HCPCS codes are among the leading causes of claim denials. These medical coding errors can happen when:
- The diagnosis code doesn’t match the procedure code.
- Outdated codes are used after annual updates.
- Unlisted or unspecified codes are used without supporting documentation.
Solution: Regular coding audits, certified coders, and updated coding software. Partnering with experts who specialize in medical billing solutions ensures coding is accurate, up-to-date, and fully compliant.
- Missing or Incomplete Information
Even small gaps in documentation, like missing provider signatures or omitted dates of service, can cause claims to be rejected.
Example: Forgetting to attach required lab results or treatment notes for certain procedures.
Solution: Create a pre-submission checklist to ensure every required field and attachment is complete before sending a medical claim to the payer.
- Eligibility and Coverage Issues
Submitting a claim for a patient whose insurance coverage has expired or who isn’t covered for that service is a guaranteed denial.
Solution: Always verify coverage before the appointment. This can be automated through eligibility verification tools integrated with your billing software.
- Duplicate Claims
Duplicate submissions can happen when staff accidentally resubmit a claim or fail to check the payer acknowledgment before re-billing.
Solution: Track claim status electronically and train staff to follow up on pending claims before resubmitting.
- Incorrect Modifiers
Modifiers are essential for indicating that a procedure was altered in some way without changing its definition. Using the wrong modifier or forgetting one entirely can result in denials.
Solution: Train coders thoroughly and keep a quick-reference guide for common modifier scenarios to reduce errors.
- Payer-Specific Requirements Not Met
Each payer has unique rules for certain procedures, documentation, or coding formats. Missing these nuances can lead to preventable denials.
Solution: Maintain a payer-specific guide and update it regularly. This ensures that every medical claims meets the requirements of the payer you’re submitting to.
- Late Submissions
Claims that miss the payer deadlines are automatically rejected. Timely filing limits vary widely, from 30 days to one year.
Solution: Automate reminders and track filing deadlines by payer to ensure on-time submissions.
- Lack of Prior Authorization
Many procedures, tests, or medications require pre-approval from the payer. Submitting without prior authorization is a costly mistake.
Solution: Have a pre-service verification workflow to confirm whether prior authorization is needed and obtain it before scheduling.
- Poor Internal Communication
When providers, billing teams, and front-desk staff aren’t aligned, vital details can be lost in the process, leading to incomplete or incorrect claims.
Solution: Streamline workflows, encourage team communication, and adopt integrated practice management software that connects clinical and billing data.
The Role of Professional Medical Billing Solutions
Preventing these common issues often comes down to having the right systems, training, and expertise in place. This is where a professional partner like DoctorPapers can make all the difference.
By combining advanced technology with skilled medical billing specialists, you can ensure:
- Accurate coding that minimizes medical coding errors.
- Timely submission and follow-up for faster payments.
- Compliance with payer-specific policies to protect revenue.
When claims are clean the first time, you get paid faster and with far less administrative hassle.
FAQs
What is a clean claim in medical billing?
A clean claim is an error-free medical claim that’s processed and paid by the payer on the first submission.
How do Medical Coding errors affect claims?
Coding errors can cause mismatches between diagnosis and procedures, leading to denials and delayed payments.
Can outsourcing help prevent claim denials?
Indeed. Expert medical billing solutions may increase claim acceptance rates, decrease mistakes, and expedite procedures.
What’s the most common reason for a claim denial?
In the U.S., eligibility issues and medical coding errors are leading causes.
How can I improve my claim approval rate?
Staff training, regular code checks, and working with a trustworthy billing source may all have a big impactct.
Conclusion: Fewer Errors, More Revenue
Despite their seeming inevitability, the majority of claim denials may be avoided with the correct approach. Healthcare providers may significantly increase clean claim rates by investing in proven medical billing solutions and addressing the underlying causes of inaccurate patient information and medical coding problems.
Your bottom line depends on it, and with the right partner, your claims process can go from stressful to seamless.






