Medical billing depends on accuracy, and one of the most important parts of the process is getting CPT codes right. These codes, which seem like random numbers to the layman, are extremely critical to physicians and their billing process. They describe the services physicians provide and determine how practices are reimbursed. In specialties like cardiology, where advanced diagnostic testing is routine, proper coding is especially important for smooth and accurate cardiology billing.
Among the most frequently used cardiology codes is CPT 93306. It’s tied to a procedure that helps detect and monitor heart conditions, making it critical for many cardiology practices. But because of its detailed requirements, this code is also a common source of billing errors. Having a thorough understanding of how to use it correctly helps physicians, coders, and practices avoid denials and keep revenue flowing smoothly.
A Detailed Look at CPT Code 93306
To understand how this code works in cardiology billing, it’s important to know what the test includes, when it’s used, and how it differs from similar codes.
What is CPT Code 93306?
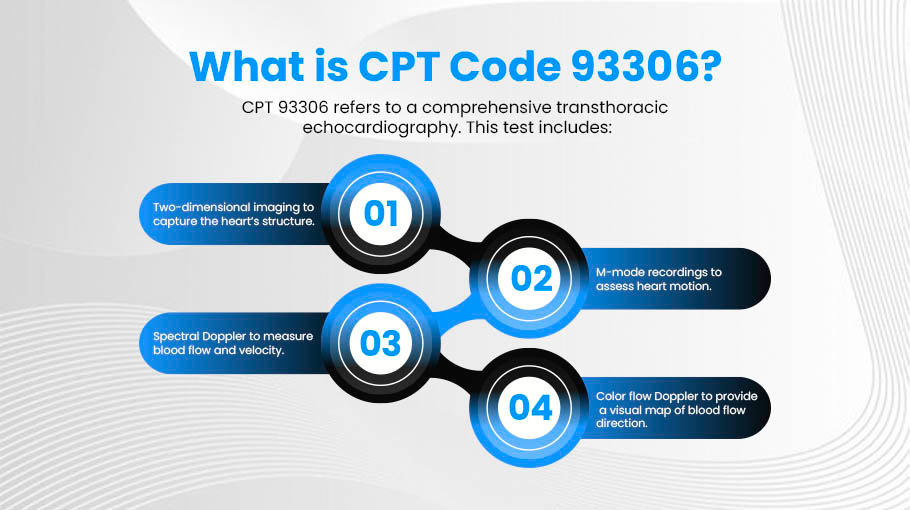
It refers to a comprehensive transthoracic echocardiography. This test includes:
- Two-dimensional imaging to capture the heart’s structure.
- M-mode recordings to assess heart motion.
- Spectral Doppler to measure blood flow and velocity.
- Color flow Doppler to provide a visual map of blood flow direction.
Together, these elements provide a full evaluation of heart structure and blood movement, making it a key diagnostic tool for cardiologists.
When Physicians Order It
Cardiologists typically order 93306 code to diagnose or monitor:
- Heart valve disorders
- Cardiomyopathy
- Congenital heart defects
- Abnormal chest pain or shortness of breath
- Unexplained changes in heart function
Because of its ability to give both structural and functional details, this test is one of the most commonly used studies in cardiology.
How 93306 Differs From Other Codes
Not every echocardiogram qualifies. Related codes include:
- 93307: A comprehensive echocardiogram without Doppler or color flow
- 93308: A limited or follow-up echocardiogram
Using 93306 when Doppler isn’t performed is one of the most common reasons claims are denied. Understanding these differences is critical for both providers and coders.
Why CPT 93306 is Important in Cardiology Billing
Given that it is such a high-volume procedure, it plays a big role in the financial health of cardiology practices. Even small errors can lead to significant losses.
Errors with this code typically fall into three main categories:
- Missing or Incomplete Documentation
If a provider does not clearly record Doppler or color flow findings, the exam does not meet the requirements of this code. Without this documentation, payers often deny the claim.
- Wrong Code Selection
Many practices mistakenly submit this code when only part of the study was performed. For example, if Doppler was not used, the correct code should be 93307. These missteps create unnecessary denials.
- Administrative Oversights
Simple mistakes, such as missing patient details, incorrect dates, or provider numbers, are also common. These may seem small, but they can delay payment just as much as coding errors.
So, what is the real cost of these mistakes?
Every denial means extra administrative work to correct and resubmit the claim. For practices handling dozens of 93306 procedures each month, repeated denials quickly add up. They can cause cash flow problems and increase the workload for billing staff. This is why accuracy in cardiology billing is so critical.
Documentation and Compliance Essentials
Payers require specific details to approve claims for this CPT code. Practices that build strong documentation habits face fewer denials.
- Complete Echocardiographic Study
The report must confirm that a full transthoracic study was performed, not just a partial or follow-up. Limited notes can raise red flags with payers.
- Doppler Evaluation
Spectral Doppler must be included, showing measurements of blood flow and velocity. Without this, the claim does not qualify as 93306.
- Color Flow Mapping
Providers must record color flow Doppler results, which visually show how blood moves through the heart chambers and valves.
- Detailed Physician Report
The physician’s report should clearly summarize findings from all components of the study. Ambiguity in notes often leads to claim rejection.
- Compliance With Payer Rules
Each insurer may have unique requirements. For example, some may require additional supporting documentation or specific modifiers. Practices that keep up with payer rules see better reimbursement outcomes.
Avoiding Common Mistakes With CPT 93306
While documentation is a big part of the challenge, there are other pitfalls practices should be aware of.
- Confusing Comprehensive and Limited Studies
Not every echocardiogram is “comprehensive.” Some providers mistakenly use it when only a limited study was done. This is one of the top reasons for denial reasons.
- Forgetting Doppler or Color Flow Results
Because these are required, forgetting to include them in the report automatically disqualifies the claim. Coders should always double-check that both are present.
- Overlooking Modifiers
Some payers require modifiers when multiple echocardiograms are done on the same day or when certain conditions apply. Omitting these can trigger denials.
- Inaccurate Patient or Provider Information
Even a small typo in a patient’s ID number or date of service can delay reimbursement. Practices should implement a verification step before claim submission.
Outsourcing Cardiology Billing Services: A Growing Need
Even with strong internal processes, billing for cardiology can get quite complicated and taxing. Codes like 93306 highlight just how detailed the requirements can be. For many practices, keeping up with documentation standards, payer rules, and constant updates becomes overwhelming.
- Outsourcing Reduces Denials
Experienced billing specialists understand the finer points of codes like 93306. They ensure that documentation matches payer expectations and that claims are submitted correctly the first time.
- Outsourcing Saves Time and Resources
For smaller practices, billing errors take staff away from patient care. By choosing outsourcing cardiology billing services, providers can reduce administrative strain and focus more on clinical work.
- Outsourcing Improves Revenue Cycle Performance
Partnering with a trusted medical billing company doesn’t just prevent mistakes. It often leads to faster payments, fewer write-offs, and better long-term financial health.
Conclusion
This CPT code is one of the most important codes in cardiology, but it comes with strict documentation and coding requirements. A lack of precision can result in denials, delays, and unnecessary work for staff. By understanding the procedure, meeting compliance standards, and avoiding common mistakes, practices can secure proper reimbursement and protect their revenue.
FAQs
- What is CPT 93306?
CPT 93306 code is a comprehensive transthoracic echocardiogram with Doppler and color flow mapping used to evaluate cardiac structure, valve function, and blood flow.
- When should CPT 93306 be billed?
It should be billed for initial or follow-up comprehensive echocardiograms that include Doppler and color flow studies.
- Can CPT 93306 be billed with a limited echocardiogram?
No, it should only be billed when a full, comprehensive study is performed. Limited echocardiograms require different CPT codes.
- What documentation is required for 93306 billing?
Complete patient history, comprehensive cardiac evaluation, Doppler and color flow findings, interpretation of abnormalities, and the performing physician’s signature.